CASE REPORT | https://doi.org/10.5005/jp-journals-10034-1093 |
Left Atrial Myxoma Causing Mitral Valve Obstruction with Right Ventricular Dysfunction Complicated by Atrial Fibrillation
1–4Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author: Krishna P Gourav, Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India, Phone: +91 8194952345, e-mail: kpgmbbs777@gmail.com
How to cite this article Kajal K, Gourav KP, Bhat I, et al. Left Atrial Myxoma Causing Mitral Valve Obstruction with Right Ventricular Dysfunction Complicated by Atrial Fibrillation. J Perioper Echocardiogr 2019;7(1):12–14.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Myxomas are the most common type of tumors of the heart and account for 83% of the primary tumors. The left atrium (LA) is the most common site for myxoma, followed by the right atrium. Obstructive symptoms of myxomas can mimic as mitral stenosis, and the severity increases due to an increase in heart rate such as the development of atrial fibrillation (AF). There is a high probability of developing pulmonary artery hypertension and right ventricular (RV) failure in patients with long-standing LA myxomas which can further be complicated by the development of AF. As the majority of patients with LA myxomas present late due to their nonspecific symptoms, a thorough assessment of pulmonary artery hypertension and RV function assessment should be done before surgical intervention.
Keywords: Atrial fibrillation, Left atrium myxoma, Right ventricular dysfunction.
INTRODUCTION
Atrial myxomas are the most common primary heart tumors.1 Majority of them found in the left atrium (LA) followed by the right atrium and commonly presents between 30 years and 60 years.2 Histologically, atrial myxomas are considered to be benign tumors; however, due to the variability in their position, they can be lethal. Bou et al. concluded that atrial fibrillation (AF) can be associated with LA myxoma with an incidence of 8.6%.3 We hereby report a case of LA myxoma with severe right ventricular (RV) dysfunction who got symptomatic due to the acute onset of AF.
CASE DESCRIPTION
A 35-year-old male patient came to our institute with a chief complaint of palpitations and grade IV dyspnoea for the last 6 hours. His blood pressure was 80/50 mm Hg and had an irregularly irregular pulse with a rate of 154/minute. On auscultation, a low-pitched grade III mid-diastolic murmur was heard at the mitral area in addition to bilateral basal crepitation. Electrocardiography showed AF with a rate of 152/minute. Transthoracic echocardiography (TTE) revealed a bi-atrial enlargement, dilated right ventricle, and a large (59 × 40 mm) mobile hyperechoic mass in the LA originating from interatrial septum which is prolapsing into the left ventricle in diastole (Figs 1A and B and Video 1). Color Doppler echocardiography revealed an increased flow velocity across the mitral valve during diastole and severe tricuspid regurgitation (TR). Right ventricular systolic pressure (RVSP) was estimated as 58 mm Hg + central venous pressure (CVP) from TR jet (Fig. 2). Tricuspid annular plane systolic excursion of the lateral wall of the tricuspid annulus was 9 mm, suggesting a severe RV dysfunction. Because of LA myxoma and grade IV dyspnea, the patient was taken for excision on an emergency basis. In the operating room after attaching the standard American Society of Anesthesiologists monitoring, an arterial line was placed in the left radial artery, a 7-French triple lumen, central venous catheter was placed in the right internal jugular vein. Anesthesia was induced with 200 μg fentanyl and 60 mg ketamine. Muscle relaxant was achieved with 6 mg vecuronium and the trachea was intubated with 8-mm endotracheal tube. Transesophageal echocardiography (TEE) probe (6VT; GE Healthcare; Vivid e9; Norway) was inserted, and the TTE findings were confirmed (Figs 1C and D). Continuous-wave Doppler placed across the mitral valve revealed a mean gradient of 13 mm Hg (Fig. 3). Anesthesia was maintained with isoflurane and with intermittent doses of vecuronium. Ventilator management was adjusted to maintain PCO2 between 30 mm Hg and 35 mm Hg and PaO2 between 100 mm Hg and 150 mm Hg. A large mass of 60 mm × 64 mm × 42 mm was successfully excised under cardiopulmonary bypass (CPB). After adequate rewarming, we tried coming off CPB with inotropic support of milrinone 0.6 μg/kg/minute, noradrenaline 0.1 μg/kg/minute, and adrenaline 0.1 μg/kg/minute. However, we could not maintain the blood pressure and the CVP raised up to 20 mm Hg. Transesophageal echocardiography showed a severe RV dysfunction with severe TR with RVSP of 65 mm Hg and CVP of 17 mm Hg (Fig. 4 and Video 2). Pulmonary artery pressure (PAP) was measured by a 26-G needle and found to be near systemic. The CPB was again initiated and inhaled nitric oxide (iNO) was started at 20 ppm in the inspiratory limb of the ventilator to prevent RV failure. After 20 minutes, the patient was successfully weaned off from CPB with stable hemodynamics. In the postoperative period, oral sildenafil was started at a dose of 0.5 mg/kg three times a day. As hemodynamics were stable with a cardiac index of 2.5 L/minute/m2, RVSP of 40 mm Hg and CVP of 6 mm Hg, iNO was tapered after 48 hours. Extubation of trachea was done 24 hours after stopping iNO, and it was uneventful. Later on, inotropic agents were reduced and stopped, and the patient was shifted to ward from the intensive care unit (ICU) after 7 days without any complication. Transthoracic echocardiography revealed a moderate RV dysfunction with good left ventricular (LV) systolic function before discharge. During the ICU stay, there were no episodes of AF, and the methemoglobin concentration never exceeded 0.9%.

Figs 1A to D: Left atrial myxoma in different echocardiographic views: (A) Apical 4-chamber view; (B) Parasternal aortic valve long axis view; (C) Midesophageal 4-chamber view; (D) Midesophageal aortic valve long axis view. AO, aorta; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle
DISCUSSION
Myxomas are the most common type of tumors of the heart and account for 83% of primary tumors.4 The LA is the most common site for myxoma, which includes 80% of all, followed by the right atrium. These tumors predominately occur in female gender with age of presentation varies from 1 month to 81 years.5 The clinical picture of atrial myxomas can be of three types, which include constitutional symptoms, obstructive symptoms, and symptoms related to tumor embolism. However, in only 5.7% of cases, myxomas are initially suspected due to its nonspecific symptoms.6 Arrhythmias can occur in atrial myxomas which include AF, atrial flutter, ventricular fibrillation, paroxysmal supraventricular tachycardia, etc.; however, these are relatively uncommon. Atrial fibrillation being the most common with an incidence of 8.6% can occur due to the size of the tumors which increases the size of the LA and increases the wall stress which, in turn, increases the susceptibility of atria to the reentrant phenomenon.3,7 Bou et al. found that patients who developed AF had a 5.1–4.3 cm mean size of myxoma; however, the correlation was not clinically significant.3 While, Koo et al. reported the role of the inflammatory process in the development of AF in LA myxoma.8
The symptoms related to obstruction of LA myxomas are mainly dependent on the tumor size, location of the tumor, and the diastolic filling time of the left ventricle. In AF, due to an increase in heart rate, diastolic filling time decreases which impair the diastolic filling into LV, and the clinical picture of LA myxoma can mimic like mitral stenosis. Pucci et al. reviewed 53 LA myxoma cases and found that the mitral stenotic effect occurs when the tumor size exceeds 5 cm.9 Keeling et al. in their study found that there is an increased risk of embolization in LA myxoma patients who had rhythm other than sinus rhythm.10 Hence, there can be an increased risk of embolization in LA myxoma patients who develop AF. In the index case, the size of the tumor was 59 × 40 cm which is relatively big to cause AF. Due to its LV inflow obstruction, LA myxomas can increase pulmonary venous pressure which, in turn, increases the load on the right ventricle leading to dilation of RV. However, the right heart enlargement was found in only 4% of LA myxoma cases.11 Nakano et al. described a positive correlation between PAP and tumor size.12 Rottlaender et al. in their study concluded that the patients with a cohort of pulmonary arterial hypertension (PAH) who developed AF had impaired New York Heart Association functional class and 6-minute walk distance when compared with PAH with sinus rhythm cohort.13 Excision of the tumor is the recommended treatment of LA myxoma, and some authors reported the reduction PAH after resection of tumor.14 However, in our case, in spite of tumor removal, the RV dysfunction and PAH persist. It may be due to the chronicity of the myxoma and elevated left atrial pressures from obstruction, causing chronic changes in pulmonary vasculature and right ventricle. With relief of the left atrial hypertension by removing LA myxoma, eventual remodeling and recovery of the right ventricle remains possible in the index case with longer term follow-up.

Fig. 2: A continuous wave Doppler was placed across tricuspid regurgitation in apical 4-chamber view
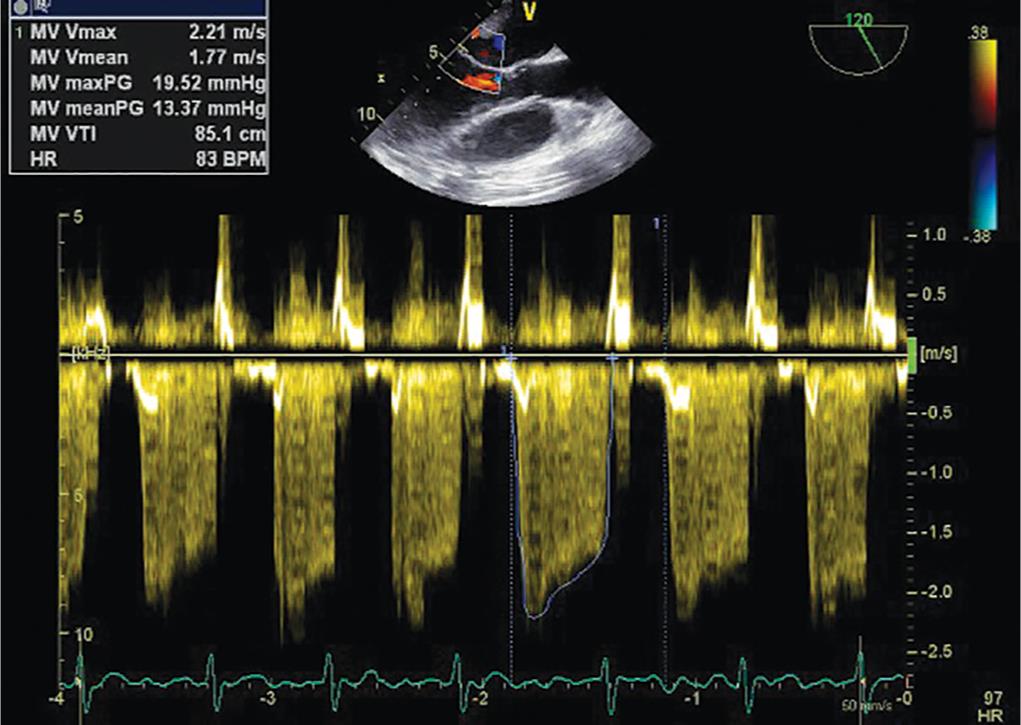
Fig. 3: A continuous wave Doppler placed across mitral valve in midesophageal long axis view showing a mean gradient of 13 mm Hg in diastole

Fig. 4: Left ventricular mid-papillary view in transesophageal echocardiography after termination of cardiopulmonary bypass showing a dilated right ventricle
In summary, obstructive symptoms of LA myxomas can mimic as mitral stenosis, and the severity can further increase due to an increase in heart rate. There is a high probability of developing pulmonary artery hypertension and RV failure in patients with long-standing LA myxomas which can further be complicated by the development of AF. As the majority of patients with LA myxomas present late due to their nonspecific symptoms, a thorough assessment of pulmonary artery hypertension and RV function is necessary before going for resection.
AUTHR CONTRIBUTIONS
Kamal Kajal, Krishna P Gourav and Imran Bhat managed the case and prepared the manuscript. Srinath Damodaran prepared the manuscript.
Video 1: Left atrial myxoma in apical 4-chamber view with severe right ventricular dysfunction
Video 2: Left ventricular mid papillary view in transesophageal echocardiography after termination of cardiopulmonary bypass showing a dilated right ventricle
REFERENCES
1. Ullah W, Mcgovern R. Natural history of an atrial myxoma. Age Ageing 2005;34(2):186–188. DOI: 10.1093/ageing/afi010.
2. Reynen K. Cardiac myxomas. New Engl J Med 1995;333(24):1610–1617. DOI: 10.1056/NEJM199512143332407.
3. Bou E, Hernández P, Cerezo L, et al. Heart tumors in Puerto Rico de novo atrial fibrillation as clinical presentation in a subgroup of patients. P R Health Sci J 2013;32(1):14–17.
4. Blondeau P. Primary cardiac tumors--French studies of 533 cases. Thorac Cardiovasc Surg 1990;38 (Suppl 2):192–195. DOI: 10.1055/s-2007-1014065.
5. Kuon E, Kreplin M, Weiss W, et al. The challenge presented by right atrial myxoma. Herz 2004;29(7):702–709. DOI: 10.1007/s00059-004-2571-7.
6. Goswami KC, Shrivastava S, Bahl VK, et al. Cardiac myxomas: clinical and echocardiographic profile. Int J Cardiol 1998;63(3):251–259. DOI: 10.1016/S0167-5273(97)00316-1.
7. Cere E, Lombardi A, Vinelli S, et al. Concomitant left atrial myxoma and atrial fibrillation in patients with peripheral embolism. Ital Heart J Suppl 2002;3(2):232–234.
8. Koo SH, Cha TJ, Choi YJ, et al. Evidence for a role of inflammation in atrial fibrillation associated with heart failure and the protective effects of angiotensin receptor blockade. Heart Rhythm 2008;5:S263.
9. Pucci A, Gagliardotto P, Zanini C, et al. Histopathologic and clinical characterization of cardiac myxoma: review of 53 cases from a single institution. Am Heart J 2000;140(1):134–138. DOI: 10.1067/mhj.2000.107176.
10. Keeling IM, Oberwalder P, Anelli-Monti M, et al. Cardiac myxomas: 24 years of experience in 49 patients. Eur J Cardiothorac Surg 2002;22(6):971–977. DOI: 10.1016/S1010-7940(02)00592-4.
11. Oliveira R, Branco L, Galrinho A, et al. Cardiac myxoma: a 13-year experience in echocardiographic diagnosis. Rev Port Cardiol 2010;29(7–8):1087–1100.
12. Nakano T, Mayumi H, Hisahara M, et al. The relationship between functional class, pulmonary artery pressure and size in left atrial myxoma. Cardiovasc Surg 1996;4(3):320–323. DOI: 10.1016/0967-2109(95)00090-9.
13. Rottlaender D, Motloch LJ, Schmidt D, et al. Clinical impact of atrial fibrillation in patients with pulmonary hypertension. PLoS One 2012;7(3): e33902. DOI: 10.1371/journal.pone.0033902.
14. Kim B-K, Cho J-N, Park H-J, et al. Reversible pulmonary hypertension in adolescent with left atrial myxoma. J Cardiovasc Ultrasound 2011;19(4):221–223. DOI: 10.4250/jcu.2011.19.4.221.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.