LETTER TO THE EDITOR | https://doi.org/10.5005/jp-journals-10034-1095 |
Post-cardiopulmonary Bypass Pacing: A Potential Pitfall in Assessment of Mitral Regurgitation
1–4Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India
5Department of Cardiothoracic and Vascular Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author: Krishna P Gourav, Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India, Phone: +91 8194952345, e-mail: kpgmbbs777@gmail.com
How to cite this article Niyogi SG, Gourav KP, Kajal K, et al. Post-cardiopulmonary Bypass Pacing: A Potential Pitfall in Assessment of Mitral Regurgitation. J Perioper Echocardiogr 2019;7(1):22–23.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Temporary pacing acts as an essential modality for maintaining hemodynamic stability in some life-threatening arrhythmias developed after cardiac surgery. We hereby discuss a case of partial balanced atrioventricular septal defect (AVSD) in which temporary pacemaker acted as a potential pitfall in the assessment of mitral regurgitation (MR). This case highlights the impact of pacing mode on MR severity and hence influencing perioperative decision-making after intracardiac repair.
Keywords: Echocardiography, Mitral regurgitation, Pacing.
Arrhythmia is one of the major causes of mortality and morbidity after cardiac surgery, especially in congenital heart disease, in patients who are vulnerable to rhythm disturbances in the early postoperative period. Temporary epicardial pacing wires are routinely placed after cardiac surgery, and temporary pacing has become a useful and an essential modality for maintaining hemodynamic stability in certain cases. We hereby discuss a case in which temporary pacing acted as a potential pitfall in the assessment of mitral regurgitation (MR).
CASE DESCRIPTION
A 5-year-old male patient presented with partial balanced atrioventricular septal defect (AVSD). The transthoracic echocardiography (TTE) showed a separate atrioventricular (AV) valves, 12 mm ostium primum atrial septal defect (ASD), and no ventricular septal defect (VSD). In addition to it, a cleft in the mitral valve was detected leading to severe MR. A mild tricuspid regurgitation (TR) with moderate pulmonary arterial hypertension was also noted in TTE. He underwent an intracardiac repair with a single-patch closure technique of ASD, and the cleft of the mitral valve was repaired after midline sternotomy under cardiopulmonary bypass (CPB) with mild hypothermia. The child developed sinus bradycardia after removing the aortic cross-clamp. Hence, a temporary epicardial right ventricular (RV) pacing wire was inserted and the RV was paced at a rate of 100 beats per minute on asynchronous ventricular pacing (VOO) mode. The patient was weaned successfully from the CPB with minimal inotropic support. Transesophageal echocardiography done post-CPB showed no residual ASD with normal biventricular function. It also revealed a severe MR with mild to moderate TR (Fig. 1; Video 1). While the possibility of inadequate surgical repair was being considered, atrial pacing lead placement was done and AV sequential pacing was commenced at the same rate on asynchronous dual chamber pacing (DOO) mode. Surprisingly, after this changeover, a reduction in the severity of MR from severe to mild was noted (Fig. 2; Video 2). The child was shifted to intensive care unit with stable hemodynamics on dual-chamber temporary pacemaker (DOO mode) pacing at a rate of 100/minute. The child later regained his normal heart rate appropriate for his age and the pacemaker was disconnected. His follow-up TTE showed a mild MR.
DISCUSSION
The influence of pacing on severity of MR has been reported in multiple cases previously1–4 and also been demonstrated in a prospective study.5 It is postulated to be due to either intra-LV dyssynchrony resulting from inversion of the physiological LV activation sequence or AV dyssynchrony from pacing, ventricle; sensing, ventricle; response; inhibited (VVI) pacing. In almost all the cases described previously, hemodynamic deterioration was observed. However, institution of proper pacing has reduced the MR and avoided the need for surgical intervention.
While most of the evidence base is from the adult population in secondary MR or valvular heart disease, a case series by Janoušek et al. has looked into the usage of cardiac resynchronization therapy in pediatric cardiomyopathy and congenital heart disease and demonstrated the same phenomena, i.e., reduction in AV valve regurgitation in a variety of anatomical substrates including systemic left ventricles, systemic right ventricles, and single-ventricle physiology.6 However, their analysis excluded regurgitation in the immediate postoperative period like in our case. Transient AV blocks and sinus bradycardia are common after CPB, especially in AVSD and VSD repair, which might have coexistent MR. Temporary epicardial pacing is often required in these patients. As seen in the index case, ventricular pacing can entail a danger of overestimation of regurgitation and might prompt an unnecessary surgical intervention.
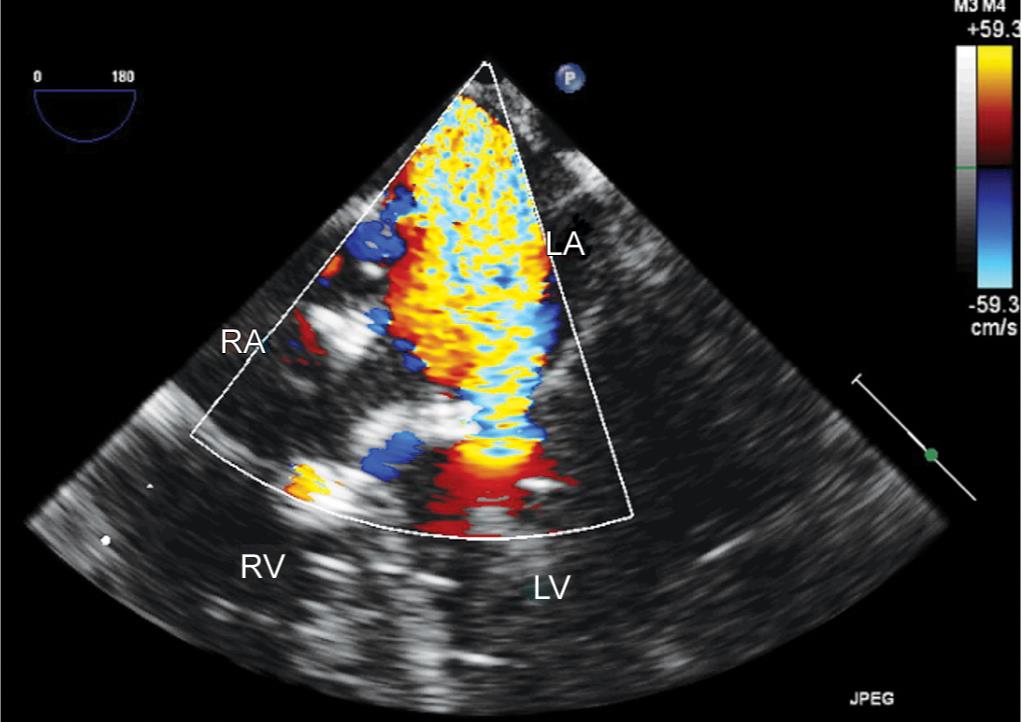
Fig. 1: Midesophageal four-chamber view showing severe MR on VOO pacing
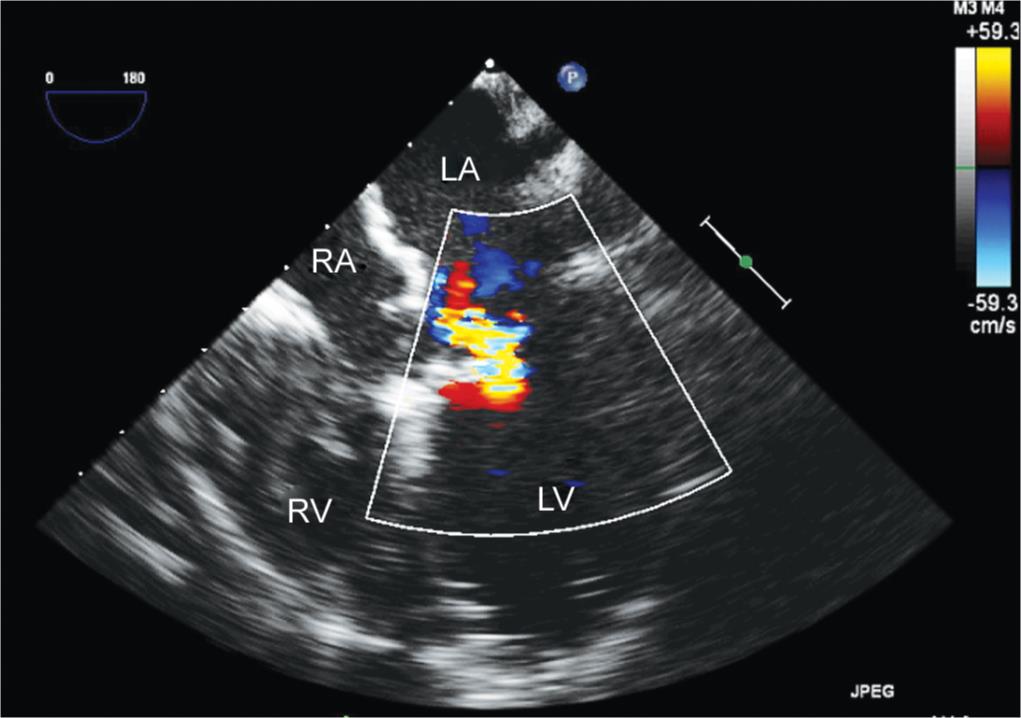
Fig. 2: Midesophageal four-chamber view showing mild MR on DOO pacing
This case highlights the importance of pacing mode in the immediate postoperative period in the setting of pediatric congenital heart surgery and mitral valve repair. This is also the first report showing the influence of pacing mode on MR severity and hence influencing perioperative decision-making in a pediatric patient. To conclude, the mode of pacing should be considered and optimized before conducting postrepair perioperative echocardiography and surgical decision-making, so as to avoid unnecessary surgical intervention.
AUTHOR CONTRIBUTIONS
Subhrashis G Niyogi, Krishna P Gourav and Rupesh Kumar managed the case and prepared the manuscript. Kamal Kajal managed the case. Sunder Negi had prepared the manuscript
Video 1: Midesophageal four-chamber view showing severe MR on VOO pacing
Video 2: Midesophageal four-chamber view showing mild MR on DOO pacing
REFERENCES
1. Wong DT, Leong DP, Khurana S, et al. Severe mitral regurgitation due to right ventricular apical pacing. BMJ Case Rep 2010;2010:1–4. DOI: 10.1136/bcr.12.2009.2524.
2. DeSimone CV, Nkomo VT, DeSimone DC, et al. An approach to the stepwise management of severe mitral regurgitation with optimal cardiac pacemaker function. Indian Pacing Electrophysiol J 2014;14(2):75–78. DOI: 10.1016/S0972-6292(16)30732-X.
3. Andrei O, Ciudin R, Ginghina C. The relationship between atrioventricular and intraventricular conduction disorders and mitral regurgitation and the impact that implantable devices have upon it. Rev Rom Cardiol 2015;25:430–438.
4. Motwani SK, Datt V, Tempe DK. Severe mitral regurgitation due to pacing in patient post aortic valve replacement (a case report). World J Cardiovasc Surg 2018;8(1):22–27. DOI: 10.4236/wjcs.2018.81003.
5. Alizadeh A, Sanati HR, Haji-Karimi M, et al. Induction and aggravation of atrioventricular valve regurgitation in the course of chronic right ventricular apical pacing. Europace 2011;13(11):1587–1590. DOI: 10.1093/europace/eur198.
6. Janoušek J, Gebauer RA, Abdul-Khaliq H, et al. Cardiac resynchronisation therapy in paediatric and congenital heart disease: differential effects in various anatomical and functional substrates. Heart 2009;95(14):1165–1171. DOI: 10.1136/hrt.2008.160465.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.