REVIEW ARTICLE | https://doi.org/10.5005/jp-journals-10034-1101 |
Role of Echocardiography in COVID-19 Patients
1–3Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author: Sunder L Negi, Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India, Phone: +91 9888446388, e-mail: dr.sundernegi@gmail.com
How to cite this article Negi SL, Gourav KP, Niyogi SG. Role of Echocardiography in COVID-19 Patients. J Perioper Echocardiogr 2019;7(2):33–35.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Coronavirus disease-2019 (COVID-19) pandemic has created new challenges for the healthcare systems all over the world. The incidence of myocardial injury ranges between 7 and 20% in hospitalized COVID-19 patients.1 The term myocardial injury applies to any patient in whom at least one cardiac troponin (cTn) concentration is above the 99th percentile upper reference limit. The death rate in COVID-19 patients with cardiac disease as comorbidity has around 10%. Myocardial injuries might be related to the fulminant cytokine release and systemic inflammation seen in severe COVID-19 cases.2 The role of echocardiographer is crucial as echocardiography is an easily available non-invasive bedside modality to assess for cardiac involvement as well as cardiorespiratory interactions in patients with COVID-19. However, sonographers are also at risk of being infected during the performance of echocardiogram, due to the prolonged and close contact with COVID-19 patients. Hence, appropriate protective measures are necessary to enable the best medical care for patients while also maintaining the health of the sonographer, especially in the setting of a shortage of expert staff (sickness or quarantine after duty) and to prevent transmission to other staff and patients. This article presents a clinical case series of a range of cardiac involvement in COVID-19 and offers guidance on indications of echocardiogram and safe practices for performing safe and effective echocardiography during the COVID-19 pandemic, with particular focus on echocardiography of suspected or confirmed COVID-19 cases. Echocardiography during COVID-19 is a clinically useful tool. Due to concerns about transmission of disease during performing an echo, the procedure should be streamlined, performed by skilled practitioners who are not at high-risk for COVID-19 severe disease, and with a focus on obtaining the best possible transthoracic images.
Keywords: Echocardiography, Ischemia, Myocardial infarction..
ECHOCARDIOGRAPHIC EXAMINATION DURATION IN CORONAVIRUS DISEASE-2019
The author has experience of echocardiographic examination in 50 coronavirus disease-2019 (COVID-19) patients admitted in intensive care unit (ICU) and HDU, mean duration required for examination is 6–9 minutes (Fig. 1). Echocardiographic calculations were performed offline. Baseline echocardiographic examinations were performed on all patients. Follow-up echo was done in COVID-19 patients based on indication, clinical information, and laboratory findings, and the progress of the underlying disease was noted.

Fig. 1: Bedside echocardiography in COVID-19 patients
CASE DESCRIPTIONS
Case 1
In COVID ICU, author received a patient with interstitial lung disease with confirmed COVID-19. Baseline echocardiography was performed which revealed normal biventricular function with mild pulmonary artery hypertension. On day 4, patient developed ST elevation in anterior leads while the cardiac biomarkers were within normal limits on multiple blood sampling (Fig. 2) and on echo, there was no evidence of regional wall motion abnormality (RWMA) (Fig. 3 and Video 1). The patient was conservatively managed, over the next 2 days ECG resolved.
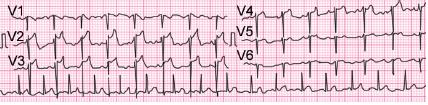
Fig. 2: 12-lead electrocardiography showing ST elevation in V2 to V4

Fig. 3: Parasternal short-axis view at mid-LV cavity level showing anterior and posterolateral wall

Fig. 4: Apical four-chamber view showing pericardial effusion
Case 2
Another patient with chronic kidney disease (CKD) was admitted to ICU with confirmed COVID-19. The patient presented with dyspnea, baseline echocardiography was performed which revealed significant pericardial effusion with the diastolic collapse of the right atrium (Fig. 4 and Video 2). Follow-up transthoracic echocardiography (TTE) was performed to see the progress of effusion. During 14 days of ICU stay, pericardial effusion was diminished in size and was discharged after becoming COVID negative.
Case 3
Another patient, baseline echocardiography was performed in view of cardiomegaly in X-ray chest which revealed severe aortic stenosis with dilated ascending aorta with LV EF 35–40%. The patient was managed medically and discharge from COVID ICU after becoming COVID negative.
Case 4
A 6-year-old male child known case of nephrotic syndrome admitted in COVID ICU with no history of ventricular dysfunction. Baseline echocardiography has shown global LV dysfunction with an ejection fraction of 35–40% (Video 3).
INDICATIONS
Echocardiography in Patients with Confirmed COVID-19 and Known Cardiac Disease
Preexisting cardiac diseases, such as, heart failure, valvular heart disease, ischemic heart disease, and hypertensive patients, are potentially aggravated by increased metabolic and hemodynamic demands in confirmed COVID-19. These patients require routine echocardiography and cardiac imaging at the bedside. However, unnecessary examinations on COVID-19 patients should be avoided to reduce the risk of contamination of personnel and misuse of resources. Indeed, careful consideration should be given to whether echocardiography and cardiac imaging will change management. The myocardial injury and the increased levels of biomarkers are likely associated with infection-induced myocarditis and ischemia. A study by Shi et al.3 found that cardiac injury in 19.7% of COVID patients was admitted in COVID ICU and the majority of patients had acute coronary artery disease.
Echocardiography in Patients with Confirmed COVID-19 with No Previous History of Cardiac Disease
A routine echocardiogram is not indicated in all patients with COVID-19 infection. Patients who are found to have elevated cardiac enzymes or abnormal electrocardiogram may be considered for an echocardiogram. Follow-up echocardiograms may be performed as clinically indicated and not at specific predefined intervals.
Echocardiography Protocol
Transthoracic echocardiography exams should be planned prior, and it should be based on clinical findings, laboratory parameters, and other imaging findings, and should be as focused to obtain diagnostic views that help in making a clinical decision. Echocardiography can help to quickly identify the circulatory status of COVID-19 patients and guide hemodynamic management. The aim would be to obtain necessary clinical information with minimum risk of exposure and to decrease the risk of contamination.4 This would be enabled by having a set protocol for baseline echo in COVID-19 patients. During the echocardiographic examination, ECG should be removed from an ultrasound machine to limit contamination and measurements should be performed offline to reduce exposure and contamination. The imaging team should be quick enough to review the echo findings and communicate them with the primary treating team for further management. Five basic views of echocardiography [apical four-chamber view, apical five-chamber view, parasternal long-axis view, parasternal short-axis view, and subcostal inferior vena cava (IVC) long-axis view] should be measured.
Left Ventricle
Global systolic function (ejection fraction), any RWMA, left ventricular outflow tract (LVOT) velocity time integral (VTI), and the end-diastolic dimension of LV.
Right Ventricle
Tricuspid annular plane systolic excursion (TAPSE), pulmonary acceleration time (PAT), and tricuspid regurgitation pressure gradient (TRP).
Valvular Assessment
Should look for color compare the view of MV and TV in apical four-chamber and parasternal long view; color compares of PV in parasternal short and long view; color compares of aortic valve in parasternal long and apical outflow tract view.
Pericardium
Look for any thickened pericardium or effusion.
Inferior Vena Cava
Subcostal view for the volume assessment.
Transesophageal echocardiography (TEE) in COVID-19 patients is associated with the high risk of contamination of equipment and healthcare workers because it can promote the aerosolization of the virus during the TEE. If TEE is clinically necessary, then would it be performed in a controlled manner with intubation with closed circuit, should be avoided in doing in awake sedation. In general, there would be very few indications for a TEE if TTE is done and has reasonable images unless the patient is undergoing cardiac surgery.
Practical Issues While Performing Echocardiography on COVID-19 Presumed/Confirmed
- Healthcare workers are at increased risk of infection while performing the echocardiographic examination, it is due to close contact involved during echocardiographic studies.
- Performing echocardiographic examination under PPE is challenging as it involves blurred vision due to fogging and sweating, difficulty in moving knobs during image acquisition and analyzing due to three-layered gloves, all these factors lead to prolongation of scan time and increases the likelihood of contamination. Scan times should be minimized by excluding inexperienced practitioners from performing imaging.
- In addition to limiting the number of echocardiography practitioners involved in scanning, it is of utmost importance to limit the exposure of staff who may be particularly susceptible to severe complications of COVID-19. Staff with age >60 years, having an underlying chronic illness, preexisting immunocompromised condition, and pregnancy should consider avoiding contact with patients presumed or confirmed to have COVID-19.
- Increased risk of contamination of equipment. Equipment care is critical in the prevention of transmission. All additional equipment (extra transducer, ECG leads) should be removed from the ultrasound system to limit exposure of the equipment. Equipment (probes and machine consoles) should be covered with disposable plastic. However, the benefit of using protective covers must be balanced against the risk of potential for suboptimal images and prolongation of scan time. Alternatively, recommended wipes that kill COVID-19 can be used to deepclean and disinfect machines after use for a patient with presumed/confirmed COVID-19.
- Single-use gel packets (not bottles) should be used in the echocardiographic examination on COVID-19 patients. If singleuse gel packets are not available, a syringe filled ultrasound gel should be used in place of the single-use packet. The gel-filled syringes can then be discarded after the exam is completed.
- The equipment should be cleaned after the exam is performed. The ultrasound equipment needs to be cleaned in entirety from top to bottom including the wheels. The use of dedicated ultrasound machines in COVID-19 patients is mandatory.
CONCLUSION
Echocardiography during COVID-19 is a clinically useful tool. Due to concerns about transmission of disease during performing an echo, the procedure should be streamlined, performed by skilled practitioners who are not at high-risk for COVID-19 severe disease, and with a focus on obtaining the best possible transthoracic images.
Video 1: Parasternal short axis view showing normally contracting LV walls
Video 2: Apical four chamber view showing significant pericardial effusion with collapsing right sided chambers
Video 3: Parasternal short axis view showing global hypokinesia of LV walls
REFERENCES
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395(10223):497–506. DOI: 10.1016/S0140-6736(20)30183-5.
2. Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395(10229):1033–1034. DOI: 10.1016/S0140-6736(20)30628-0.
3. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5(7):802–810. DOI: 10.1001/jamacardio.2020.0950.
4. Neskovic AN, Skinner H, Price S. Focus cardiac ultrasound core curriculum and core syllabus of the European association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging 2018;19(5):475–481. DOI: 10.1093/ehjci/jey006.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.