CASE REPORT | https://doi.org/10.5005/jp-journals-10034-1113 |
Pneumomediastinum and Pneumopericardium: Impediment to the Transthoracic Echo Windows
1–3Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author: Thanigai Arasu, Department of Anesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India, Phone: +91 9862520701, e-mail: thani9894252525@gmail.com
How to cite this article Arasu T, Negi SL, Puri GD. Pneumomediastinum and Pneumopericardium: Impediment to the Transthoracic Echo Windows. J Perioper Echocardiogr 2020;8(1):18–20.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Aim and objective: To highlight the impediments for the transthoracic echo windows.
Background: Pneumomediastinum and pneumopericardium with cardiac A-lines obscuring the transthoracic echo windows.
Case description: A 57-year-old male patient with COVID-19 infection underwent tracheostomy and positive pressure ventilation following which he developed pneumomediastinum/pneumopericardium. Subsequently, the apical and parasternal cardiac windows replaced by A-lines hindering the echocardiographic examination.
Conclusion: The disappearance of the previously available echo window should raise the suspicion of new-onset pneumomediastinum or pneumopericardium.
Keywords: Cardiac A-lines, COVID-19, Pneumomediastinum, Pneumopericardium.
BACKGROUND
Pneumomediastinum and pneumopericardium are defined as the presence of air or gas in the mediastinal space and pericardial sac, respectively, and it commonly occurs secondary to chest trauma and positive pressure ventilation or even spontaneously.1 COVID-19 pandemic contributed to the increased number of such cases may be in part of alveolar damage.2 Generally, it does not impose any clinical threat unless massive, yet, it can hinder the transthoracic echocardiogram examination due to the presence of intervening air which is a poor conductor of ultrasound waves. Here, we report and discuss one such case of pneumomediastinum and pneumopericardium in a post-COVID acute respiratory distress syndrome (ARDS) patient with cardiac A-lines obscuring the transthoracic echo windows.
CASE DESCRIPTION
History: A 57-year-old male COVID-positive patient was admitted to our hospital with complaints of fever, shortness of breath, and chest pain. He was on oxygen support initially. Subsequently, he got intubated and put on mechanical ventilation and received standard COVID care protocol. Echo was done to evaluate the cause of chest pain and as a routine examination revealed normal examination.
He underwent a tracheostomy because of difficult weaning, the following day he had hemodynamic instability. ECG showed sinus tachycardia (Fig. 1). Standard echo windows could not be obtained in the repeat echo performed to evaluate the cause of hemodynamic instability. Apical and parasternal windows were filled with A-lines (Fig. 2). Through the subcostal window, cardiac function was evaluated which seemed to be normal.
Repeat chest X-ray (CXR) showed consolidations and pneumomediastinum (Fig. 3).
High-resolution computed tomography (HRCT) chest was done to rule out any fungal cavities and confirmed the presence of cavities along with additional findings of pneumomediastinum/pneumopericardium (Fig. 4).
In due course patient deteriorated clinically despite maximum interventions, subsequently, the patient expired.
DISCUSSION
Pneumomediastinum occurs commonly due to trauma when alveoli rupture leads to escape of air dissecting the bronchoalveolar sheath and entering into the mediastinum called Macklin effect.3 Among the traumatic causes, airway instrumentation and positive pressure ventilation are the important iatrogenic trigger4 and it is most often treated conservatively with supportive measures and close monitoring with goals of symptoms relief.5

Fig. 1: ECG showed sinus tachycardia
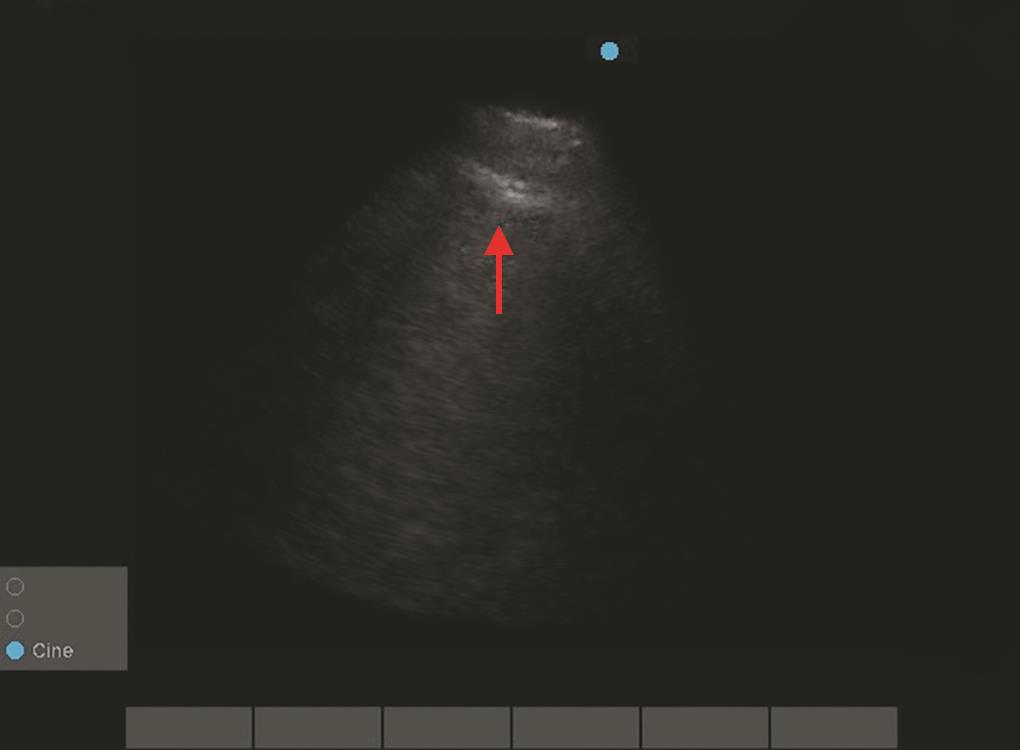
Fig. 2: Echo image showed A-lines in apical, parasternal long-axis, parasternal short-axis view Echo image showed A-lines in apical, parasternal long axis, parasternal short-axis view
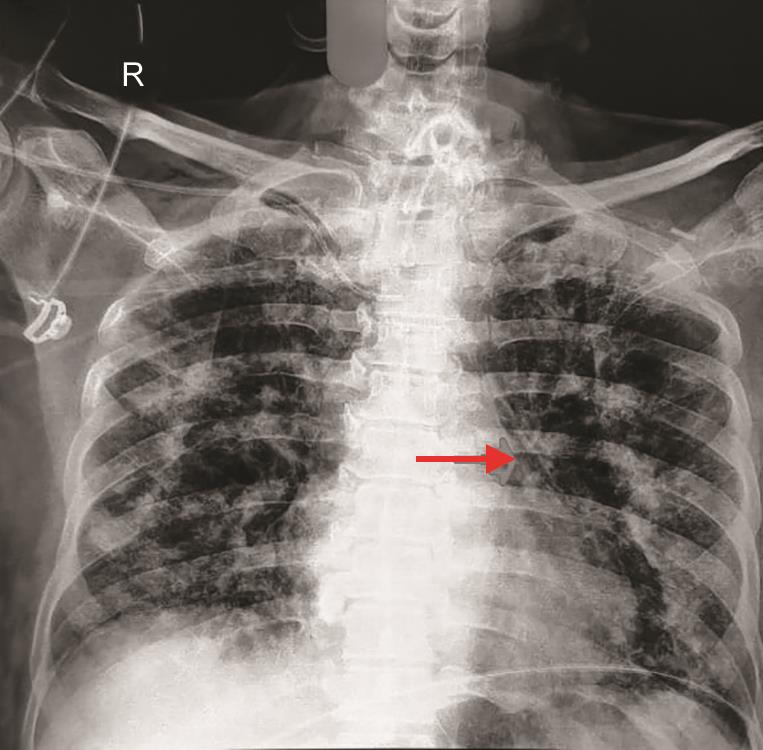
Fig. 3: CXR showed multifocal patchy consolidations, fibrotic bands in bilateral lungs and pneumomediastinum

Fig. 4: HRCT showed areas of ground glass opacity, patchy consolidations, fibrotic bands, and tractional bronchiectasis diffusively involving bilateral lung cavities. Pneumomediastinum/pneumopericardium are also noted
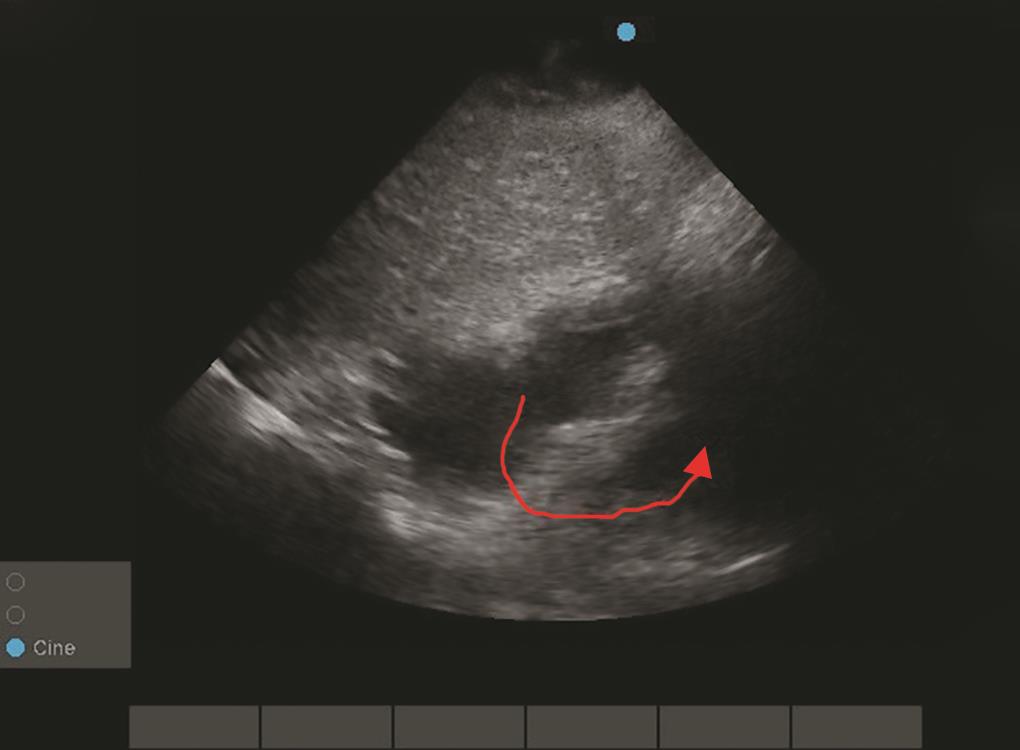
Fig. 5: Echo image showed air gap sign in subxiphoid view. In diastole the air was displaced showing both ventricles
Pneumopericardium can occur de novo following trauma including barotrauma or it may simply be an extension from pneumomediastinum in which air from the mediastinum gain entry along the venous channels where the pericardial reflections are weak.6
Following the COVID-19 pandemic, the number of patients requiring intubation and or tracheostomy and need for mechanical ventilation due to ARDS has surged, so thus the risk of pneumomediastinum and also dysregulated inflammation in COVID-19 causes myocarditis and to some extent, it can cause pericarditis also, this could potentially sever the barrier between pericardium and mediastinum leading to pneumopericardium in case if the air was present in the mediastinum.7
This viral-induced myocarditis causes poor LV function and it can be easily diagnosed by point of care 2D echocardiography in the form of global hypokinesia before biomarkers availability.8 Also, echo is the bedside tool for evaluation of volume status and to diagnose pulmonary embolism which is quite common among COVID-19 patients. So, serial echocardiography is vital in intensive care settings in this COVID era.
The presence of air in the mediastinum or pericardium can hinder the echocardiographic window and the sudden disappearance of the previously available window should raise the suspicion of the presence of pneumomediastinum and or pneumopericardium. In those conditions, transesophageal echocardiography (TEE) may be a good alternative to evaluate heart functions.
Usually, pneumomediastinum or pneumopericardium is diagnosed by HRCT. However, replacement of echo windows by cardiac A-lines (Fig. 2) and air gap sign (Fig. 5), almost pointing out the presence of intervening air,9 and its extent with the exact site of window replaced by A-lines can interpret the location of air to a certain extent.
In pneumomediastinum, the contact between the pericardium and the diaphragm still remains even though there is a collection of mediastinal air surrounding the heart, so the subcostal view allows for echocardiographic visualization of the heart in pneumomediastinum. However, the presence of free air in the abdomen or a large gastric bubble may obscure this view.10
Collections of air within the pericardium can completely obstruct visualization of the heart on echocardiogram including subcostal window,11 but if only a small amount of air is found within the pericardium then the view may only be partially obscured.12
The other conditions to consider on the differential for air on the parasternal and apical windows include pneumothorax, severe COPD.10
CONCLUSION
The disappearance of the previously available echo window should raise the suspicion of new-onset pneumomediastinum or pneumopericardium.
Although pneumomediastinum and pneumopericardium are benign entities of little clinical significance its presence is hindering the routine transthoracic echo examination in ICU settings which may be vital for the patients and necessitates invasive TEE for the particular patient.
REFERENCES
1. Kouritas VK, Papagiannopoulos K, Lazaridis G, et al. Pneumomediastinum. J Thorac Dis 2015;7 (Suppl 1):44–49. DOI: 10.3978/j.issn.2072-1439.2015.01.11.
2. Belleti A, Palumbo D, Zangrillo A, et al. Predictors of pneumothorax/pneumomediastinum in mechanically ventilated covid-19 patients. J Cardiothorac Vasc Anesth 2021;35(12):3642–3651.
3. Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944;23(4):281–358. DOI: 10.1097/00005792-194412000-00001.
4. Sahni S, Verma S, Grullon J, et al. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci 2013;5(8):460–464. DOI: 10.4103/1947-2714.117296.
5. Perna V, Vilà E, Guelbenzu JJ, et al. Pneumomediastinum: is this really a benign entity? when it can be considered as spontaneous? Our experience in 47 adult patients. Eur J Cardiothorac Surg 2010;37(3):573–575. DOI: 10.1016/j.ejcts.2009.08.002.
6. Mansfield PB, Granam CB, Beckwith JB, et al. Pneumopericardium and pneumomediastinum in infants and children. J Pediatr Surg 1973;8(5):691–699. DOI: 10.1016/0022-3468(73)90408-9.
7. Shah JZ, Kumar SA, Patel AA. Myocarditis and pericarditis in patients with COVID-19. Heart Views 2020;21(3):209–214. DOI: 10.4103/HEARTVIEWS.HEARTVIEWS_154_20.
8. Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm 2020;17(9):1463–1471. DOI: 10.1016/j.hrthm.2020.05.001.
9. Reid CL, Chandraratna PAN, Kawanishi D, et al. Echocardiographic detection of pneumomediastinum and pneumopericardium: the air gap sign. J Am Coll Cardiol 1983;1(3):916–921. DOI: 10.1016/s0735-1097(83)80209-5.
10. Zachariah S, Gharahbaghian L, Perera P, et al. Spontaneous pneumomediastinum on bedside ultrasound: case report and review of the literature. West J Emerg Med 2015;16(2):321–324. DOI: 10.5811/westjem.2015.1.24514.
11. Allgood NL, Brownlee JR, Green GA. Inability to view the heart through the subxiphoid echocardiographic window: a harbinger of disaster. Pediatr Cardiol 1994;15(1):27–29. DOI: 10.1007/BF00797002.
12. Md Noor J, Eddie EA. Cardiac A-lines in fast scan as a sign of pneumopericardium. Ultrasound J 2019;11(1):7. DOI: 10.1186/s13089-019-0123-x.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.